What is Achilles Tendinopathy?
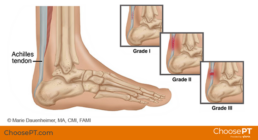
Your Achilles tendon, which is the thickest tendon in your body, connects your calf muscles to your heel bone (calcaneus). You use this tendon when you perform activities like walking, running, and jumping. A sudden increase, overuse, in the amount or intensity of activities like these can cause the tendon to become stressed and inflamed. You may have one of two types of tendinopathies depending on which part of your tendon is swollen. If you have non-insertional achilles tendinopathy, which usually affects young active people, the fibers in the middle of your tendon have torn causing swelling and pain. If you have insertional achilles tendonitis, fibers have torn in the lower part of the tendon where it connects to the heel bone. This often causes bone spurs (an extra growth of bone) to develop.
Symptoms
- Pain in the achilles tendon in the morning or first few steps after sitting
- Tenderness to the touch
- Swelling of the tendon (you can often feel a bump)
- Feeling of calf tighness
- Bone spur associated with insertional tendonitis
If you experienced a “popping” sensation in the back of your heel or if your pain is persistent, you may have ruptured your achilles tendon. A physical therapist is trained to diagnose the severity of your condition, and if surgery is a likely outcome, they will refer you to the appropriate surgeon.
Treatment
Physical therapy is a very important resource for treating Achilles Tedinopathy, especially for those suffering from non-insertional tendonitis. Your physical therapist will aim to reduce pain and swelling in the area and increase your strength, flexibility, and control. Physical therapists are trained to assess your situation and create a recovery plan that’s specific to your needs. Below are some examples of what you can expect:
- Heat/Ice treatment
- Soft tissue mobilization
- Joint mobilization
- Mobility training
- Progressive resistance exercise
- Proprioception & balance exercises
The therapist will also provide you with a specialized home exercise program and teach you to perform the exercises correctly ensuring the quickest recovery.
Your physical therapist can also help you safely ease back into your prior activities at the right time. He or she may recommend orthotics (custom or over the counter) or heel lifts in order to help you find relief as your recover.
If your pain doesn’t improve after six months of conservative treatment, your physical therapist may recommend a physician to evaluate your need for surgery. The doctor will recommend a specific type of surgery based on which part of your tendon is injured and how bad the tear is. If you choose to have surgery, physical therapy will play an important role in your recovery after the operation. It may take a full year of post-surgical treatment until you can return to full physical activity pain-free.
Physical Therapy Exercises
The following are examples of exercises you may be prescribed in a physical therapy clinic. Please remember these do not apply to everyone and depend on your specific condition.
- Ankle Circles: Stand up straight and elevate your injured foot by flexing the knee. Slowly circle your foot in the air for 30 seconds and repeat.
- Calf Stretch: While standing, face a wall and place your hands against it as you lean forward. Keep affected leg’s knee straight and place the unaffected leg in front with the knee bent. Push your hips toward the wall and hold for 45 seconds. Relax and repeat. You should feel a strong stretch in your calf.
- Sitting Heel/Toe Raise: Sit on a chair and rise up onto your toes as high as you can without pain. Lower heels slowly and gently lift up your toes. Repeat.
- Standing Heel Raise: Stand up straight and rise up onto your toes using both feet. Lift up your nonaffected leg and then slowly control your lowering down with the the affected leg only. Repeat.
Prevention
Follow the guidelines listed below in order to help prevent Achilles Tendinopathy:
- Walk for a few minutes and complete a dynamic warm-up before running.
- Do calf-strengthening exercises weekly.
- Stretch your calf muscles and achilles tendon.
- Increase your level of activity gradually.
- Alternate high impact activities (like running) with low-impact activities (like cycling).
- Wear supportive shoes, and limit time in high heels.
Think you might be dealing with an Achilles Tendinopathy? Interested in preventive care? Contact MTS for an hour long 1-on-1 evaluation with a PT to get started!


This article was fantastic. You have an interesting writing style, and the data you presented is invaluable. The analysis and examples were so thorough that they were easy to follow. Your creation of this amazing resource is greatly appreciated.
Your blog post made me see [topic] in a whole new light. Thank you for broadening my perspective.
gabung sekarang di situs toto togel terpercaya, https://oiald.unimen.ac.id/data/ daftar
Daftar Resmi Sekarang Juga toto slot Terpercaya
Daftar Resmi Sekarang Juga monperatoto Terpercaya
Daftar Resmi Sekarang Juga slot mahjong Terpercaya
Reading your essay was a true pleasure for me. Your presentation style was clear and concise, and the insights you offered were priceless. Your study and writing of this are greatly appreciated. For those curious about this subject, it’s an excellent resource.
Daftar Resmi Sekarang Juga situs togel resmi Terpercaya
أنابيب الألمنيوم في العراق يتفوق مصنع إيليت بايب في توفير أنابيب الألمنيوم عالية الجودة في العراق. معروفة بخفتها وخصائصها المقاومة للتآكل، تعد أنابيب الألمنيوم لدينا مثالية لمجموعة من التطبيقات، من البناء إلى النقل. تضمن طرق الإنتاج المتقدمة المستخدمة في مصنع إيليت بايب أن تكون أنابيب الألمنيوم لدينا قوية وموثوقة، تلبي متطلبات مختلف الصناعات. كاسم رائد في القطاع، تظل مصنع إيليت بايب مكرسة لتقديم منتجات متفوقة وخدمة استثنائية. لمزيد من التفاصيل حول أنابيب الألمنيوم لدينا، يرجى زيارة موقعنا الإلكتروني على ElitePipe Iraq.
başakşehir elektrikçi Google SEO ile doğru anahtar kelimeleri kullanarak müşteri kitlesine daha kolay ulaştık. https://www.royalelektrik.com/
Great article! Your insights are very valuable, and the way you broke down the information made it easy to understand. I appreciate the time and effort you put into researching and writing this. It’s a great resource for anyone looking to deepen their understanding of the subject.
kağıthane elektrikçi Google SEO ile web sitemizin trafiği gözle görülür şekilde arttı. http://www.royalelektrik.com/istanbul-elektrikci/
başakşehir elektrikçi Google SEO sayesinde müşteri memnuniyetimiz arttı. http://royalelektrik.com/istanbul-elektrikci/
büyükçekmece elektrikçi Google SEO sayesinde müşteri tabanımızı genişlettik. http://www.royalelektrik.com/istanbul-elektrikci/
What a great story! I’m so glad you shared it. The data you supplied was both practical and simple to grasp. Your ability to simplify otherwise difficult ideas is much appreciated. Anyone interested in learning more about this subject would benefit greatly from reading this.
LDPE Pipes in Iraq Elite Pipe Factory in Iraq offers a comprehensive range of LDPE pipes, which are valued for their flexibility, lightweight nature, and resistance to various chemicals. Our LDPE pipes are engineered to meet high standards of quality, ensuring reliable performance across various applications. Recognized as one of the best and most reliable pipe manufacturers in Iraq, Elite Pipe Factory is committed to delivering products that combine durability with performance. For more information on our LDPE pipes, visit elitepipeiraq.com.
Son çıkan filmler HD indir SEO ile Google sıralamalarında yükselmek harika bir duygu. Profesyonel destek almak şart! http://royalelektrik.com/
Vergisiz alkol Google SEO, dijital pazarlama stratejimizde büyük bir fark yarattı. http://royalelektrik.com/
Awesome! Its genuinely remarkable post, I have got much clear idea regarding from this post
I am truly thankful to the owner of this web site who has shared this fantastic piece of writing at at this place.
Your post is really helpful and based on solid research. The material you supplied is quite beneficial, and your writing style is captivating. Your inclusion of concrete instances is quite helpful. Anyone interested in learning more about this subject would benefit greatly from reading this.
Great Article bro, situs togel resmi daftar sekarang
Daftar Resmi Sekarang Juga situs togel resmi Terpercaya
Daftar Resmi Sekarang Juga situs toto Terpercaya
Excellent piece! Your thorough summary is much appreciated. I now see the issue from a different angle thanks to your insightful comments. You made your points quite clearly with the examples you included. You have my gratitude for penning this.
Daftar Resmi Sekarang Juga toto togel Terpercaya
Makanan mengandung bahan berbahaya Borak
Daftar Resmi Sekarang Juga situs toto Terpercaya
Daftar Resmi Sekarang Juga https://prisma.pupuk-indonesia.com/file/ Terpercaya
Daftar Resmi Sekarang Juga situs toto login Terpercaya
This article was incredibly insightful! Your detailed explanations and well-organized content made it easy to follow along. I appreciate the practical examples you included, as they really helped to illustrate your points. Thank you for sharing such valuable information.
Nice post. I learn something totally new and challenging on websites
Daftar bandar togelsitus toto Terpercaya
Daftar bandar togelsitus toto Terpercaya
Great Article bro, taik itu enak
selamat datang di situs togel terbaik, situs toto resmi
selamat datang di situs togel terbaik, situs toto resmi
Great information shared.. really enjoyed reading this post thank you author for sharing this post .. appreciated
Very well presented. Every quote was awesome and thanks for sharing the content. Keep sharing and keep motivating others.
I do not even understand how I ended up here, but I assumed this publish used to be great
Daftar bandar togelsitus toto Terpercaya
selamat datang di togel online terbaik, situs togel terpercaya dan resmi
Daftar bandar togeltogel Terpercaya
Daftar bandar togelcabe4d Terpercaya
I truly appreciate your technique of writing a blog. I added it to my bookmark site list and will
selamat datang di togel online terbaik, https://tp.fkip.ulm.ac.id/toto/ terpercaya dan resmi
Joint Genesis Reviews, Pricing, and bonuses visit here: joint genesis
Great Article bro, monperatoto login daftar sekarang
Joint Genesis Reviews, Pricing, and bonuses visit here: joint genesis
Joint Genesis Reviews, Pricing, and bonuses visit here: joint genesis
Trafik manipülasyonu Google SEO sayesinde web sitemin trafiği büyük ölçüde arttı. Kesinlikle öneririm! http://royalelektrik.com/esenyurt-elektrikci/
Joint Genesis Reviews, Pricing, and bonuses visit here: joint genesis
Hello there, we are the biggest and also the best situs toto in Indonesia, I really loved your articles.
Daftar situs toto terbaik disitus togel Terpercaya
selamat datang di togel online terbaik, https://pilrek.unri.ac.id/toto/ terpercaya dan resmi
Hello there, we are the biggest and also the best situs togel in Indonesia, I really loved your articles.
Daftar resmi situs toto disitus toto login Terpercaya
Great Article bro, taik itu enak
selamat datang di togel online terbaik, situs toto resmi dan terpercaya
selamat datang di togel online terbaik, situs toto resmi dan terpercaya
Daftar resmi situs toto dislot gacor Terpercaya
selamat datang di togel online terbaik, situs togel resmi dan terpercaya
selamat datang di situs slot terbaik, situs toto daftar
Takipçi satışı Google SEO sayesinde müşteri tabanımızı genişlettik. http://www.royalelektrik.com/esenyurt-elektrikci/
selamat datang di situs slot terbaik, slot gacor daftar
selamat datang di situs slot terbaik, situs slot daftar
Family Dollar very informative articles or reviews at this time.
selamat datang di situs slot terbaik, slot tergacor daftar
selamat datang di situs slot terbaik, hongkong lotto daftar
Henof I do not even understand how I ended up here, but I assumed this publish used to be great
Daftar sekarang resmi situs toto disitus toto Terpercaya
selamat datang di togel online terbaik, https://megakemayoran.com/produk/ resmi dan terpercaya
selamat datang di togel online terbaik, https://pilrek.unri.ac.id/toto/ resmi dan terpercaya
Pink Withney Hi there to all, for the reason that I am genuinely keen of reading this website’s post to be updated on a regular basis. It carries pleasant stuff.
selamat datang di togel online terbaik, https://tp.fkip.ulm.ac.id/toto/ resmi dan terpercaya
Daftar sekarang resmi situs ditoto togel Terpercaya
bokep memek bau scam
selamat datang di togel online terbaik, situs toto resmi dan terpercaya
selamat datang di togel online terbaik, https://elibrary.sulteng.bawaslu.go.id/file/kerja/ resmi dan terpercaya
selamat datang di togel online terbaik, slot gacor resmi dan terpercaya
selamat datang di situs slot terbaik, mahjong slot daftar
selamat datang di situs slot terbaik, situs toto slot daftar
Your blog post made me see [topic] in a whole new light. Thank you for broadening my perspective.
selamat datang di situs slot terbaik, situs toto 4d daftar
Daftar sekarang resmi situs ditoto slot Terpercaya
Joint Genesis Reviews, Pricing, and bonuses visit here: joint genesis
I truly appreciate your technique of writing a blog. I added it to my bookmark site list and will
Hello there, we are the biggest and also the best situs toto in Indonesia, I really loved your articles.
Joint Genesis Reviews, Pricing, and bonuses visit here: joint genesis
Hızlı ve güvenilir takipçi SEO optimizasyonu, dijital pazarlama hedeflerimize ulaşmamıza yardımcı oldu. https://royalelektrik.com//esenyurt-elektrikci/
Düşük oturum süresi SEO ile Google sıralamalarında yükselmek harika bir duygu. Profesyonel destek almak şart! http://www.royalelektrik.com/beylikduzu-elektrikci/
selamat datang di situs slot online, slot online daftar
I just wanted to say how much I enjoyed reading your blog post. It’s rare to find such well-researched content that’s also a pleasure to read.
Hi there to all, for the reason
Reading your essay was a true pleasure for me. You were quite successful in elucidating the subject, and your writing is both interesting and easy to understand. The principles were much easier to grasp after reading the examples you provided. Your expertise is much appreciated.
This post is excellent! Your detailed analysis and engaging writing style make it a pleasure to read. I learned a lot from this article and will definitely be referring back to it in the future. Thank you for sharing your expertise with us.
This is my first time pay a quick visit at here and i am really happy to read everthing at one place
Pretty! This has been a really wonderful post. Many thanks for providing these details.
Good post! We will be linking to this particularly great post on our site. Keep up the great writing
Daftar sekarang resmi situs ditoto slot Terpercaya
Daftar sekarang resmi situs dijacktoto Terpercaya
selamat datang di situs slot terbaik, situs toto daftar
selamat datang di situs slot terbaik, hongkong lotto daftar
selamat datang di situs slot terbaik, link gacor daftar
I really value the information you’ve shared here.
Excellent job on this article! Your thorough research and engaging writing style make it a must-read for anyone interested in the topic. I appreciate the practical examples you included, as they really helped to illustrate your points. Thank you for sharing such valuable information.
Daftar sekarang resmi situs disitus slot Terpercaya
Daftar sekarang resmi situs disitus toto Terpercaya
Daftar sekarang resmi situs dihttps://balebengong.id/file/ Terpercaya
I love how thorough you were in covering this topic.
What is a good dental health? My website: prodentim reviews
Düşük oturum süresi SEO hizmetleri ile Google sıralamalarında ciddi bir artış sağladık. https://royalelektrik.com//esenyurt-elektrikci/
Gizli metin Google SEO sayesinde müşteri memnuniyetimiz arttı. https://www.royalelektrik.com/beylikduzu-elektrikci/
sumatra slim belly tonic reviews: sumatra slim belly tonic reviews
İçerik paylaşımı Google SEO sayesinde web sitemin trafiği büyük ölçüde arttı. Kesinlikle öneririm! http://www.royalelektrik.com/esenyurt-elektrikci/
Daftar prediksi togelsyair hk Terpercaya
Daftar prediksi togelhttps://tulamben.desa.id/data/ Terpercaya
This was a refreshing take on the topic, thanks!
Daftar prediksi togelsitus toto login Terpercaya
Organik hit SEO çalışmaları, web sitemizin performansını iyileştirdi. http://www.royalelektrik.com/beylikduzu-elektrikci/
hilang kau, hilang kau hilang kau
Fantastic site Lots of helpful information here I am sending it to some friends ans additionally sharing in delicious And of course thanks for your effort
hilang kau, lenyapkan hilang kau
sumatra slim belly tonic reviews: sumatra slim belly tonic reviews
dari muka dunia, hilang kau dari muka bumi
sumatra slim belly tonic reviews: sumatra slim belly tonic reviews
dari muka dunia, musnah dari muka bumi
dari muka dunia, hilang kau dari muka bumi
dari muka dunia, sampai jumpa dari muka bumi
Thank you for this fantastic article. Your insights are very valuable, and the way you presented the information made it easy to follow. I appreciate the effort you put into researching and writing this. It’s a great resource for anyone looking to learn more about this subject.
great articlejacktoto Terpercaya
great articlesitus togel Terpercaya
sumatra slim belly tonic reviews: sumatra slim belly tonic reviews
sumatra slim belly tonic reviews: sumatra slim belly tonic reviews
This is such a well-balanced and thoughtful post.
Takipçi kazanma Google SEO, web sitemizin performansını artırmak için mükemmel bir yol. https://www.royalelektrik.com//esenyurt-elektrikci/
VIP takipçi SEO hizmetleri, Google’da üst sıralarda yer almamıza yardımcı oldu. https://royalelektrik.com//beylikduzu-elektrikci/
sumatra slim belly tonic reviews: sumatra slim belly tonic reviews
great articletoto slot Terpercaya
great articlesitus toto Terpercaya
nagano tonic: nagano tonic
Sınırsız takipçi Google SEO ile hedef kitlemize daha kolay ulaşıyoruz. http://royalelektrik.com/esenyurt-elektrikci/
Sosyal medya büyüme SEO sayesinde Google’da rakiplerimizi geride bıraktık. https://royalelektrik.com//esenyurt-elektrikci/
Thanks for explaining this in such simple terms!
nagano tonic: nagano tonic
great articlesitus toto Terpercaya
great articlesitus toto Terpercaya
great articlemonperatoto Terpercaya
Üsküdar gider açıcı Üsküdar daki tuvalet tıkanıklığı için aradık, hemen geldiler ve temiz çalıştılar. https://bence.net/read-blog/231
nagano tonic: nagano tonic
شركة Bwer هي أحد الموردين الرئيسيين لموازين الشاحنات ذات الجسور في العراق، حيث تقدم مجموعة كاملة من الحلول لقياس حمولة المركبات بدقة. وتغطي خدماتها كل جانب من جوانب موازين الشاحنات، من تركيب وصيانة موازين الشاحنات إلى المعايرة والإصلاح. تقدم شركة Bwer موازين شاحنات تجارية وموازين شاحنات صناعية وأنظمة موازين جسور محورية، مصممة لتلبية متطلبات التطبيقات الثقيلة. تتضمن موازين الشاحنات الإلكترونية وموازين الشاحنات الرقمية من شركة Bwer تقنية متقدمة، مما يضمن قياسات دقيقة وموثوقة. تم تصميم موازين الشاحنات الثقيلة الخاصة بهم للبيئات الوعرة، مما يجعلها مناسبة للصناعات مثل الخدمات اللوجستية والزراعة والبناء. سواء كنت تبحث عن موازين شاحنات للبيع أو الإيجار أو التأجير، توفر شركة Bwer خيارات مرنة لتناسب احتياجاتك، بما في ذلك أجزاء موازين الشاحنات والملحقات والبرامج لتحسين الأداء. بصفتها شركة مصنعة موثوقة لموازين الشاحنات، تقدم شركة Bwer خدمات معايرة موازين الشاحنات المعتمدة، مما يضمن الامتثال لمعايير الصناعة. تشمل خدماتها فحص موازين الشاحنات والشهادات وخدمات الإصلاح، مما يدعم موثوقية أنظمة موازين الشاحنات الخاصة بك على المدى الطويل. بفضل فريق من الخبراء، تضمن شركة Bwer تركيب وصيانة موازين الشاحنات بسلاسة، مما يحافظ على سير عملياتك بسلاسة. لمزيد من المعلومات حول أسعار موازين الشاحنات، وتكاليف التركيب، أو لمعرفة المزيد عن مجموعة موازين الشاحنات ذات الجسور وغيرها من المنتجات، تفضل بزيارة موقع شركة Bwer على الإنترنت على bwerpipes.com
nagano tonic: nagano tonic
nagano tonic: nagano tonic
Üsküdar kameralı gider temizleme Üsküdar da lavabo tıkanıklığı için aradık, ekip hemen gelip sorunu çözdü. https://melds.eu/blogs/6295/%C3%9Csk%C3%BCdar-WC-T%C4%B1kan%C4%B1kl%C4%B1%C4%9F%C4%B1-A%C3%A7ma
This was a very enlightening read, much appreciated!
selamat datang di situs slot terbaik, https://ojs.uninus.ac.id/api/ daftar
+ Тащите всё на себе, нет времени на жизнь
+ Не можете построить долгие отношения, проще без них,
партнёры всё время не те
+ Испытываете эмоциональное и/или физическое выгорание
+ Испытываете эмоциональное и/или физическое
выгорание
+ В конфликте с родителями, общение холодное или
его нет вовсе
+ Не можете построить долгие отношения, проще
без них, партнёры всё время не те
+ Делаете результаты через преодоление и страдания
+ Достигли дна — долги, проблемы в
отношениях, зависимости
+ Испытываете эмоциональное и/или
физическое выгорание
+ Одиноки, нет друзей и сложно строить отношения с людьми
+ Не можете построить долгие отношения, проще без них,
партнёры всё время не те
+ Чувствуете, что страсть и любовь ушли из отношений
+ Делаете результаты через преодоление и страдания
+ Тащите всё на себе, нет времени на
жизнь
+ Не можете построить долгие отношения, проще без них, партнёры
всё время не те
https://t.me/s/psyholog_online_just_now
great articlecabe4d Terpercaya
What i dont understood is in reality how youre now not really a lot more smartlyfavored than you might be now Youre very intelligent You understand therefore significantly in terms of this topic produced me personally believe it from a lot of numerous angles Its like women and men are not interested except it is one thing to accomplish with Woman gaga Your own stuffs outstanding Always care for it up
great articledata hk Terpercaya
selamat datang di situs slot terbaik, https://umcced.edu.my/toto/ daftar
Daftar Beberapa Harga Borak
You’re so awesome! I don’t believe I have read a single thing like that before. So great to find someone with some original thoughts on this topic. Really.. thank you for starting this up. This website is something that is needed on the internet, someone with a little originality!
great articletoto Terpercaya
For the reason that the admin of this site is working, no uncertainty very quickly it will be renowned, due to its quality contents.
great articletoto slot Terpercaya
great articlesitus toto Terpercaya
selamat datang di situs slot terbaik, https://sih3.kepriprov.go.id/ daftar
great articlecabe4d Terpercaya
List beberapa orang yang ber Pala Botak
great articlepafiagamkota.org Terpercaya
great articlemonperatoto Terpercaya
great articlesyair hk Terpercaya
selamat datang di bandar togel online terbaik, toto macau resmi dan terpercaya
great articletoto slot Terpercaya
You’re so awesome! I don’t believe I have read a single thing like that before. So great to find someone with some original thoughts on this topic. Really.. thank you for starting this up. This website is something that is needed on the internet, someone with a little originality!
I really value the information you’ve shared here.
great articlebandar togel Terpercaya
Hi there to all, for the reason
great articlemonperatoto Terpercaya
I found this really easy to follow and understand.
Technoob I do not even understand how I ended up here, but I assumed this publish used to be great
Technoob Pretty! This has been a really wonderful post. Many thanks for providing these details.
This is really interesting, You’re a very skilled blogger. I’ve joined your feed and look forward to seeking more of your magnificent post. Also, I’ve shared your site in my social networks!
BYU Cougars I very delighted to find this internet site on bing, just what I was searching for as well saved to fav
systeme io: https://systemee.systeme.io
SocialMediaGirls Hi there to all, for the reason that I am genuinely keen of reading this website’s post to be updated on a regular basis. It carries pleasant stuff.
Your clear and thorough explanation made a big difference for me.
Nitric boost ultra reviews : https://nitricboostultrareviews.usaloves.com
selamat datang di situs toto slot, toto slot daftar
Fran Candelera I very delighted to find this internet site on bing, just what I was searching for as well saved to fav
great articlecabe4d Terpercaya
great articlesitus togel Terpercaya
Nitric boost ultra reviews : https://nitricboostultrareviews.usaloves.com
Nitric boost ultra reviews : https://nitricboostultrareviews.usaloves.com
Nitric boost ultra reviews : https://nitricboostultrareviews.usaloves.com
Nitric boost ultra reviews : https://nitricboostultrareviews.usaloves.com
Nitric boost ultra reviews : https://nitricboostultrareviews.usaloves.com
selamat datang di bandar togel online terbaik, situs togel resmi dan terpercaya
selamat datang di bandar togel online terbaik, toto slot resmi dan terpercaya
This is such a comprehensive post—well done!
Nitric boost ultra reviews : https://nitricboostultrareviews.usaloves.com
Nitric boost ultra reviews : https://nitricboostultrareviews.usaloves.com
Nitric boost ultra reviews : https://nitricboostultrareviews.usaloves.com
great articlejembut kuda Terpercaya
great articlejembut kuda Terpercaya
LINK SITUS SLOT GACOR DEPOSITE 5000 WD BERAPUN DI BAYAR LNK DAFTAR/
I’m always looking for content like this—thanks!
selamat datang di situs toto slot, toto togel Daftar
selamat datang di situs toto slot, situs toto Daftar
great articlebandar togel Terpercaya
bokep memek bau scam
great articlemonperatoto Terpercaya
SITUS SLOT GACOR SCATTER HITAM 2024 LNK DAFTAR/
I’ve learned a lot from this article—great job!
Sugar defender reviews : sugar defender reviews
selamat datang di situs toto slot, slot gacor Daftar
selamat datang di situs toto slot, toto slot Daftar
selamat datang di situs togel resmi, situs toto Daftar
“This article is really informative and well-written!”
I feel much more confident on this topic now, thanks!
great articlemonperatoto Terpercaya
selamat datang di bandar togel online terbaik, situs togel resmi dan terpercaya
selamat datang di situs togel resmi, situs toto macau Daftar
Sugar defender reviews : sugar defender reviews
great articlebandar togel resmi Terpercaya
SITUS SLOT GACOR SCATTER HITAM 2024 LNK DAFTAR/
AGEN SITUS SLOT GACOR SCATTER HITAM 2024 LINK DAFTAR/
selamat datang di bandar togel online terbaik, toto togel resmi dan terpercaya
selamat datang di situs togel terpercaya, toto togel Daftar
You’ve covered this subject very thoroughly—great job!
Sugar defender reviews : sugar defender reviews
I loved as much as you will receive carried out right here The sketch is attractive your authored material stylish nonetheless you command get got an impatience over that you wish be delivering the following unwell unquestionably come more formerly again since exactly the same nearly a lot often inside case you shield this hike
“Great content, learned a lot from this post!”
selamat datang di slot gacor maxwin terbaik, slot gacor resmi dan terpercaya
https://neighbourhood-london.com/
This is going to be super helpful for me.
You’ve captured the essence of the topic perfectly.
great articlejembut kuda Terpercaya
selamat datang di situs terbaik, phising
great articlesitus togel Terpercaya
selamat datang di situs togel terpercaya, situs togel Daftar
Sugar defender reviews : sugar defender reviews
Your blog post resonated with me on so many levels. It’s comforting to know that others share my perspective on this topic.
Thinker Pedia This was beautiful Admin. Thank you for your reflections.
Thinker Pedia For the reason that the admin of this site is working, no uncertainty very quickly it will be renowned, due to its quality contents.
Thinker Pedia Very well presented. Every quote was awesome and thanks for sharing the content. Keep sharing and keep motivating others.
You’ve done a great job simplifying this concept.
Your blog post was like a ray of sunshine on a cloudy day. Thank you for brightening my mood!
Website Slot Online Server Thailand Terbaik Menyediakan Provider PG Soft untuk Permainan Slot Gacor Maxwin Mahjong Ways 1, 2, dan 3, dengan Bonus Event Scatter Hitam yang Sangat Populer di Indonesia. LINK DAFTAR/
Situs Slot Gacor Maxwin Hari Ini Gampang Menang Terbaru Link Slot88 Online
Website Slot Online Server Thailand Terbaik Menyediakan Provider PG Soft untuk Permainan Slot Gacor Maxwin Mahjong Ways 1, 2, dan 3, dengan Bonus Event Scatter Hitam yang Sangat Populer di Indonesia. LINK DAFTAR
great articlengentot nungging Terpercaya
Mangaclash Nice post. I learn something totally new and challenging on websites
great articlengentot nungging Terpercaya
SLOT RAFFI AHMAD dan 3, dengan Bonus Event Scatter Hitam yang Sangat Populer di Indonesia. LINK DAFTAR
Strands Hint You’re so awesome! I don’t believe I have read a single thing like that before. So great to find someone with some original thoughts on this topic. Really.. thank you for starting this up. This website is something that is needed on the internet, someone with a little originality!
Lois Sasson This is my first time pay a quick visit at here and i am really happy to read everthing at one place
great articlesitus toto Terpercaya
selamat datang di bandar togel terbaik, toto macau resmi dan terpercaya
Your blog post was so thought-provoking. It’s rare to find content that challenges me to think deeply about important issues.
I’m always impressed with how clearly you explain things—thank you.
Your passion for this topic is contagious! After reading your blog post, I can’t wait to learn more.
Isla Moon I am truly thankful to the owner of this web site who has shared this fantastic piece of writing at at this place.
Newtoki I like the efforts you have put in this, regards for all the great content.
I love how you dive deep into the subject—great work!
FinTech ZoomUs There is definately a lot to find out about this subject. I like all the points you made
great articlemonperatoto Terpercaya
I’m definitely bookmarking this for later!
Your writing is like a breath of fresh air in the often stale world of online content. Your unique perspective and engaging style set you apart from the crowd. Thank you for sharing your talents with us.
great articlemonperatoto Terpercaya
nagano tonic reviews : nagano tonic reviews
This was an engaging read—thanks for posting!
nagano tonic reviews : nagano tonic reviews
great articlengentot nungging Terpercaya
nagano tonic reviews : nagano tonic reviews
nagano tonic reviews : nagano tonic reviews
nagano tonic reviews : nagano tonic reviews
Ümraniye teknik servis Çekiş gücü kaybolmuştu, servis sonrası toparladı. http://cocapal.com/read-blog/5191
nagano tonic reviews : nagano tonic
nagano tonic reviews : nagano tonic
nagano tonic reviews : nagano tonic
you are in reality a good webmaster The website loading velocity is amazing It sort of feels that youre doing any distinctive trick Also The contents are masterwork you have done a fantastic job in this topic
Ümraniye süpürge filtre satın al Evde temizlik sırasında süpürgem bozuldu, hemen geldiler. https://www.momcuddle.com/questions/question/elektrik-supurgesi-servisi/
elektrikli süpürge sorun çözme Servis kalitesinden çok memnun kaldım. https://frenzay.com/blogs/14481/Elektrikli-S%C3%BCp%C3%BCrge-Tamiri
süpürge servisi randevu Cihazımı ertesi gün teslim aldım, harikalar! https://social.web2rise.com/read-blog/4138
great articleslot mahjong Terpercaya
Your passion for your subject matter shines through in every post. It’s clear that you genuinely care about sharing knowledge and making a positive impact on your readers. Kudos to you!
Situs slot server luar negri terbaik bonus 100% diawal.
Situs gacor andalan yang selalu berikan pola slot gacor gampang menang terbaik hingga wd 100%
great articlejembut kuda Terpercaya
SLOT RAFFI AHMAD dan 3, dengan Bonus Event Scatter Hitam yang Sangat Populer di Indonesia. LINK DAFTAR
Thank you for the good writeup It in fact was a amusement account it Look advanced to far added agreeable from you However how could we communicate
Your blog has become an indispensable resource for me. I’m always excited to see what new insights you have to offer. Thank you for consistently delivering top-notch content!
Mountsinai Hi there to all, for the reason that I am genuinely keen of reading this website’s post to be updated on a regular basis. It carries pleasant stuff.
Mountsinai naturally like your web site however you need to take a look at the spelling on several of your posts. A number of them are rife with spelling problems and I find it very bothersome to tell the truth on the other hand I will surely come again again.
Hey there You have done a fantastic job I will certainly digg it and personally recommend to my friends Im confident theyll be benefited from this site
“This article is really informative and well-written!”
su kaçak arıza tespiti İstanbul Eyüp su kaçağı tespiti: Eyüp’te su kaçaklarını teknolojik cihazlarla buluyoruz. https://cosplaygoals.com/ustaelektrikci
selamat datang di bandar togel terbaik, toto togel resmi dan terpercaya
I found this really easy to follow and understand.
Ataşehir su kaçağı tespiti Levent su kaçağı tespiti: Levent’te su kaçağını en hızlı ve doğru şekilde tespit ediyoruz. https://kryza.network/ustaelektrikci
Pengalaman main yang seru
Beyoğlu su kaçağı tespit cihazı Zeytinburnu’nda su kaçağı tespiti için çok iyi bir ekip. Sorunumuzu hemen çözdüler. https://edenhazardclub.com/ustaelektrikci
Your blog is a treasure trove of knowledge! I’m constantly amazed by the depth of your insights and the clarity of your writing. Keep up the phenomenal work!
Avcılar su kaçağı tespiti Büyükçekmece su kaçağı tespiti: Büyükçekmece’de su kaçağı sorunlarını profesyonelce çözmekteyiz. https://cloutapps.com/ustaelektrikci
great articleanak lonte Terpercaya
Keamanan akun terjamin
Göztepe su kaçağı tespiti Bağcılar su kaçağı tespiti: Bağcılar’daki su kaçağı sorunlarına çözüm sunuyoruz. https://www.cloufan.com/ustaelektrikci
Bakırköy su tesisat kaçak tespiti Beyoğlu’ndaki evimdeki su kaçağını bulmaları çok zor oldu ama cihazları çok etkiliydi. https://aubameyangclub.com/ustaelektrikci
great articlejembut kuda Terpercaya
Fatih su kaçağı tespiti Beşiktaş’ta su kaçağı tespiti için kesinlikle doğru adres! Profesyonel hizmet. https://redsocial.cl/ustaelektrikci
selamat datang di bandar togel terbaik, toto togel resmi dan terpercaya
Hi there it’s me, I am also visiting this webb site
regularly, thios website is reallly pleasaht annd tthe vieewers arre actuaslly
sharing gopod thoughts.
İstanbul tesisat kaçak tespiti Sarıyer’deki villa için profesyonel su kaçağı tespiti hizmeti aldık, kesinlikle öneririm. https://sociofans.com/ustaelektrikci
Koza su kaçak tespiti Evimde su sızıntısı olduğunu bile fark etmemiştim, hızlıca buldular! https://snupto.com/ustaelektrikci
Bahçelievler su kaçak tespiti Caddebostan su kaçağı tespiti: Caddebostan’da su kaçağı tespitinde uzman ekip. http://socialnetwork.linkz.us/ustaelektrikci
“Mind = blown! 🌟 This is exactly the comprehensive breakdown I needed. Your expertise shines through in every paragraph. Thanks for sharing such well-researched content.”
Sırapınar su kaçak tespiti Hızlı ve kaliteli bir hizmet, tekrar ihtiyaç duyarsam ararım. https://menagerie.media/ustaelektrikci
Viagra * Cialis * Levitra
All the products you are looking suitable are currently at one’s disposal as far as something 1+1.
4 more tablets of an individual of the following services: Viagra * Cialis * Levitra
https://pxman.net
Superb, what a web site it is! This website provide helpful datta to us,
keeep it up.
شركة Bwer هي أحد الموردين الرئيسيين لموازين الشاحنات ذات الجسور في العراق، حيث تقدم مجموعة كاملة من الحلول لقياس حمولة المركبات بدقة. وتغطي خدماتها كل جانب من جوانب موازين الشاحنات، من تركيب وصيانة موازين الشاحنات إلى المعايرة والإصلاح. تقدم شركة Bwer موازين شاحنات تجارية وموازين شاحنات صناعية وأنظمة موازين جسور محورية، مصممة لتلبية متطلبات التطبيقات الثقيلة. تتضمن موازين الشاحنات الإلكترونية وموازين الشاحنات الرقمية من شركة Bwer تقنية متقدمة، مما يضمن قياسات دقيقة وموثوقة. تم تصميم موازين الشاحنات الثقيلة الخاصة بهم للبيئات الوعرة، مما يجعلها مناسبة للصناعات مثل الخدمات اللوجستية والزراعة والبناء. سواء كنت تبحث عن موازين شاحنات للبيع أو الإيجار أو التأجير، توفر شركة Bwer خيارات مرنة لتناسب احتياجاتك، بما في ذلك أجزاء موازين الشاحنات والملحقات والبرامج لتحسين الأداء. بصفتها شركة مصنعة موثوقة لموازين الشاحنات، تقدم شركة Bwer خدمات معايرة موازين الشاحنات المعتمدة، مما يضمن الامتثال لمعايير الصناعة. تشمل خدماتها فحص موازين الشاحنات والشهادات وخدمات الإصلاح، مما يدعم موثوقية أنظمة موازين الشاحنات الخاصة بك على المدى الطويل. بفضل فريق من الخبراء، تضمن شركة Bwer تركيب وصيانة موازين الشاحنات بسلاسة، مما يحافظ على سير عملياتك بسلاسة. لمزيد من المعلومات حول أسعار موازين الشاحنات، وتكاليف التركيب، أو لمعرفة المزيد عن مجموعة موازين الشاحنات ذات الجسور وغيرها من المنتجات، تفضل بزيارة موقع شركة Bwer على الإنترنت على bwerpipes.com
BWER is Iraq’s premier provider of industrial weighbridges, offering robust solutions to enhance efficiency, reduce downtime, and meet the evolving demands of modern industries.
sugar defender reviews : sugar defender
sugar defender reviews : sugar defender
sugar defender reviews : sugar defender
sugar defender reviews : sugar defender
sugar defender reviews : sugar defender
Serving Iraq with pride, BWER supplies high-performance weighbridges designed to improve transport logistics, reduce inaccuracies, and optimize industrial processes across all sectors.
sugar defender reviews : sugar defender
sugar defender reviews : sugar defender
sugar defender reviews : sugar defender
sugar defender reviews : sugar defender
Glue Dream strain Great information shared.. really enjoyed reading this post thank you author for sharing this post .. appreciated
gluco6 reviews : https://gluco6reviews.usaloves.com/
gluco6 reviews : https://gluco6reviews.usaloves.com/
gluco6 reviews : https://gluco6reviews.usaloves.com/
gluco6 reviews : https://gluco6reviews.usaloves.com/
gluco6 reviews : https://gluco6reviews.usaloves.com/
gluco6 reviews : https://gluco6reviews.usaloves.com/
gluco6 reviews : https://gluco6reviews.usaloves.com/
gluco6 reviews : https://gluco6reviews.usaloves.com/
Baddiehub I like the efforts you have put in this, regards for all the great content.
Pentru cei care cauta asistenta contabila, Lorand Expert ofera un sprijin de incredere. Cu noi, ve?i economisi timp ?i ve?i evita erorile, avand la dispozi?ie o echipa dedicata pentru toate aspectele contabile.
NY weekly Very well presented. Every quote was awesome and thanks for sharing the content. Keep sharing and keep motivating others.
NY weekly There is definately a lot to find out about this subject. I like all the points you made
Чистота и уют с gorodhim.ru
С gorodhim.ru вы получаете идеальную чистоту мягкой мебели . Химчистка диванов, кресел и стульев проводится с использованием передовых технологий и безопасных средств . Мы обеспечим качественное удаление мочи и сложных загрязнений .
Услуги химчистки для вашего дома и офиса обеспечивают выезд мастеров в удобное время . Глубокая химчистка матрасов выполняется в соответствии с высокими стандартами качества . Gorodhim.ru предоставляет услуги по доступным ценам .
Городская химчистка предлагает комплексный подход к чистоте вашего интерьера . Глубокая чистка мягкой мебели и матрасов проходит с максимальной тщательностью. Услуги нашей химчистки доступны в любой точке Москвы и области.
Современные решения от новых МФО: все мфо и мкк без отказов и проверок. Ставка фиксирована — 1% в день, доступно каждому.
Попробуйте свою удачу в лучших онлайн казино, где ставки высоки.
Попробуйте свои силы вместе с нами, и получите незабываемые впечатления.
Выберите свое любимое казино онлайн, и начните играть уже сегодня.
Почувствуйте атмосферу настоящего казино в режиме онлайн, не покидая своего уютного кресла.
Ставьте на победу с нашими играми, и покажите всем, кто здесь главный.
Насладитесь игровым процессом вместе с игроками со всех уголков планеты, и станьте лучшим из лучших.
Играйте и выигрывайте, получая щедрые бонусы, которые увеличат ваши шансы на победу.
Играйте и наслаждайтесь азартом в каждой ставке, и погрузитесь в мир бесконечных перспектив.
Станьте частью казино онлайн и получите доступ к эксклюзивным играм, с минимум затрат времени и усилий.
онлайн казино казино онлайн беларусь .
Остекление балконов по выгодной цене в Петербурге, поможем выбрать подходящий вариант.
Профессиональное остекление балконов в Петербурге, по доступным ценам и с гарантией качества.
Индивидуальное остекление балконов в СПб, под заказ и с уникальным дизайном.
Надежное остекление балконов в СПб, без скрытых платежей и срочно.
Экономичное остекление для балконов в Санкт-Петербурге, со скидками и акциями.
остекление балкона спб цена https://balkon-spb-1.ru/ .
1 доллар в тенге 1 юань в тенге .
Получите доступ к актуальным курсам валют с любым устройством. Конвертация тенге, рублей и других валют на сайте происходит мгновенно, а удобный интерфейс делает процесс максимально простым.
Качественные натяжные потолки в Санкт-Петербурге|Экономьте на натяжных потолках в Санкт-Петербурге|Профессиональная установка натяжных потолков в СПб|Огромный ассортимент натяжных потолков в Санкт-Петербурге|Как выбрать идеальный натяжной потолок в СПб|Натяжные потолки в Петербурге для вашего уюта|Современный дизайн с натяжными потолками в Санкт-Петербурге|Натяжные потолки в СПб: лучший выбор для вашего дома|Долговечные и стойкие натяжные потолки в Санкт-Петербурге|Технологичные решения для натяжных потолков в Санкт-Петербурге|Быстрое и качественное установление натяжных потолков в Санкт-Петербурге|Идеальный выбор: натяжные потолки в СПб|Инновации и креативность в сфере натяжных потолков в Санкт-Петербурге|Специальные предложения на натяжные потолки в Петербурге|Натяжные потолки в СПб: выбор современных людей|Экспертный подход к натяжным потолкам в Петербурге|Комфорт и эстетика с натяжными потолками в Санкт-Петербурге|Профессиональный подход к выбору и установке натяжных потолков в Санкт-Петербурге|Уникальный дизайн вашего потолка: натяжные потолки в Санкт-Петербурге|Плюсы натяжных потолков в Петербурге|Технологические новинки для натяжных потолков в Санкт-Петербурге|Премиальный сервис по установке натяжных потолков в СПб|Новинки в оформлении потолков: натяжные потолки в Петербурге|Оптимальный выбор: натяжные потолки в Петербурге
натяжные потолки петербург https://potolki-spb-1.ru/ .
Noodlemagazine I really like reading through a post that can make men and women think. Also, thank you for allowing me to comment!
Noodlemagazine There is definately a lot to find out about this subject. I like all the points you made
Players rave about Taya365’s live casino, which replicates the excitement of a real-life casino. Interact with live dealers in real-time while enjoying games like blackjack and roulette.
taya365 slot taya365 casino login .
Hoi, dit is een reactie.
Om te beginnen met beheren, bewerken en verwijderen van reacties, ga je naar het Reacties scherm op het dashboard. https://pxman.net
Noodlemagazine naturally like your web site however you need to take a look at the spelling on several of your posts. A number of them are rife with spelling problems and I find it very bothersome to tell the truth on the other hand I will surely come again again.
Профессиональная откачка канализации в Слуцке, эффективно.
Оперативная откачка канализации в Слуцке, по выгодной цене.
Профессиональные услуги по откачке канализации в Слуцке, с опытными специалистами.
Актуальные услуги откачки канализации в Слуцке, с оперативным выездом.
Служба откачки канализации в Слуцке: оперативное решение проблем, по круглосуточно.
Оперативная откачка канализации в Слуцке: круглосуточно, с выездом в любую точку города.
Экстренная откачка канализации в Слуцке: оперативно и качественно, с использованием современного оборудования.
Профессиональная откачка канализации в Слуцке: надежно и оперативно, с быстрым выездом на объект.
Откачка канализации в Слуцке: оперативно и качественно, по доступной цене.
откачка туалетов Слуцк откачка канализации Слуцк .
Noodlemagazine I do not even understand how I ended up here, but I assumed this publish used to be great
I loved as much as you will receive carried out right here The sketch is tasteful your authored subject matter stylish nonetheless you command get got an edginess over that you wish be delivering the following unwell unquestionably come further formerly again as exactly the same nearly very often inside case you shield this hike
Лучшие советы по выбору металлической входной двери, которая прослужит долгие годы.
Места, где можно приобрести качественную входную металлическую дверь.
Как не ошибиться с выбором входной металлической двери.
Преимущества металлических входных дверей перед другими видами.
купить входную дверь заказать входную дверь .
В чем отличия входных металлических дверей разных производителей.
Секреты успешной покупки входной металлической двери, идеально впишется в интерьер.
Места, где можно приобрести качественную входную металлическую дверь.
Как не ошибиться с выбором входной металлической двери.
5 основных причин купить металлическую входную дверь.
входная дверь дверь металлическая .
Как выбрать между дверью одного бренда и дверью другого.
Лучшее казино для аркадных игр | Новые аркадные игры каждую неделю | Победите в аркадах и станьте миллионером | Играйте в аркады и выигрывайте деньги | Онлайн казино с самыми популярными аркадными играми | Уникальные аркады только у нас | Играйте в аркады и наслаждайтесь выигрышами | Увлекательные аркады и возможность заработать деньги | Лучшие аркадные развлечения для вас | Увлекательные аркады для ценителей азарта | Онлайн казино с увлекательными аркадами | Новые аркадные развлечения каждый день | Побеждайте в аркадах и станьте миллионером | Аркадные развлечения и азарт вместе | Выигрывайте крупные суммы в аркадных играх | Побеждайте в аркадных играх и получайте призы
arkada casino играть бонус код arkada casino .
Секреты успешной покупки входной металлической двери, идеально впишется в интерьер.
Места, где можно приобрести качественную входную металлическую дверь.
входная дверь дверь металлическая .
Что учесть при выборе входной металлической двери.
Почему стоит выбрать металлическую входную дверь.
Как выбрать между дверью одного бренда и дверью другого.
Играйте в аркадные игры в лучшем онлайн казино | Уникальные аркадные игры только здесь | Увлекательные аркадные игры и безграничный азарт | Азартные аркады и огромные выигрыши | Новый уровень азарта в онлайн казино | Соберите комбинации и побеждайте в аркадах | Играйте в аркады и наслаждайтесь выигрышами | Играйте в аркады и выигрывайте деньги | Играйте в аркадные игры и ощутите азарт | Увлекательные аркады для ценителей азарта | Онлайн казино с увлекательными аркадами | Выигрывайте крупные суммы в аркадах | Аркадные онлайн развлечения для вас | Лучшие аркадные развлечения только у нас | Побеждайте в аркадах и получайте денежные призы | Побеждайте в аркадных играх и получайте призы
arkada casino промокод за регистрацию arkada вход .
Лучшее казино для аркадных игр | Играйте в эксклюзивные аркады в онлайн казино | Онлайн казино для ценителей аркадных игр | Азартные аркады и огромные выигрыши | Играйте в увлекательные аркады и выигрывайте призы | Соберите комбинации и побеждайте в аркадах | Уникальные аркадные игры ждут вас | Азарт и аркады в одном месте | Уникальные аркадные развлечения только здесь | Играйте в аркадные игры и выигрывайте деньги | Аркадные игры для всех желающих азарта | Побеждайте в аркадных баталиях и зарабатывайте деньги | Испытайте свою удачу в аркадном казино | Увлекательные аркады и возможность заработать крупные суммы | Уникальные аркадные игры в онлайн казино | Побеждайте в аркадных играх и получайте призы
arkada casino бонусы для новичков arkada casino актуальное зеркало .
Играйте в аркадные игры в лучшем онлайн казино | Играйте в аркадные игры и выигрывайте крупные призы | Попробуйте свою удачу в аркадном казино | Азартные аркады и огромные выигрыши | Онлайн казино с самыми популярными аркадными играми | Большие выигрыши в аркадных играх | Азартные аркады для всех желающих | Играйте в аркады и выигрывайте деньги | Онлайн казино с удивительными аркадными играми | Онлайн казино с азартными аркадами | Играйте в лучшие аркады и выигрывайте призы | Побеждайте в аркадных баталиях и зарабатывайте деньги | Побеждайте в аркадах и станьте миллионером | Лучшие аркадные развлечения только у нас | Аркадные развлечения для всех | Увлекательные аркады и возможность заработать деньги
arkada casino рабочее зеркало arkada casino бонус .
Умный способ управления жалюзи, облегчит вашу жизнь.
Снижайте затраты на отопление и кондиционирование воздуха с автоматизацией жалюзи.
Удобное управление жалюзи через интернет.
Повысьте уровень безопасности с автоматическими жалюзи.
Качественное обслуживание автоматизированных жалюзи.
жалюзи с автоматикой https://elektrokarniz18.ru/ .
Лучшие решения для автоматизации жалюзи, повысит комфорт в помещении.
Экономьте энергию с помощью автоматики для жалюзи.
Контролируйте жалюзи с помощью смартфона.
Создайте уютную атмосферу с автоматическими жалюзи.
Профессиональная установка автоматики для жалюзи.
жалюзи роллеты автоматика https://elektrokarniz18.ru/ .
Идеальный привод для жалюзи.
с помощью привода.
Как выбрать правильный привод для жалюзи.
Плюсы использования привода для жалюзи.
Тенденции в автоматизации жалюзи с помощью привода.
Как управлять жалюзями с помощью смартфона с использованием привода.
Секреты успешной установки привода для автоматизации жалюзей.
Экономьте время и энергию с автоматизированным приводом для жалюзи.
Забавные истории об использовании приводов для жалюзей.
Почему привод для жалюзи делает жизнь легче и удобнее.
жалюзи с приводом жалюзи с приводом .
Необычные электрокарнизы для вашей сцены, которые удивят зрителей.
Электрокарнизы – стильное решение для сцены, делая представление более динамичным.
Управляйте световыми шоу с помощью электрокарнизов, дарят возможность воплотить любую идею.
Лучшие электрокарнизы для профессиональных выступлений, с идеальным сочетанием функциональности и эстетики.
Создайте неповторимую магию на сцене с электрокарнизами, с непревзойденным качеством и надежностью.
Превратите ваше шоу с помощью электрокарнизов, которые способны изменить восприятие аудитории.
Электрокарнизы – лучший выбор для сцены, с легкой и тихой работой в каждом представлении.
Осуществите свои идеи с помощью электрокарнизов, для тех, кто стремится к совершенству.
Трансформируйте свой спектакль с электрокарнизами, и подчеркивая профессионализм исполнителей.
Идеальные решения для любого жанра и формата, чтобы сделать шоу неповторимым и запоминающимся.
как выбрать электрокарниз для театра https://elektrokarniz8.ru/ .
Необычные электрокарнизы для вашей сцены, которые удивят зрителей.
Электрокарнизы придают шоу утонченность, позволяя создать эффектные декорации.
Современные технологии в электрокарнизах, и незабываемым для зрителей.
Электрокарнизы помогут создать атмосферу шоу, для тех, кто ценит качество и стиль.
Лучшие электрокарнизы для вашего шоу, с непревзойденным качеством и надежностью.
Сверхсовременные технологии в каждом дизайне, которые способны изменить восприятие аудитории.
Освежите свое шоу с электрокарнизами, и создадут неповторимую атмосферу.
С электрокарнизами ваша сцена станет настоящим шедевром, способных придать умиротворение или напряжение вашему выступлению.
Трансформируйте свой спектакль с электрокарнизами, воплощая самые смелые идеи в жизнь.
Идеальные решения для любого жанра и формата, обеспечив себе идеальный результат в каждом выступлении.
автоматический карниз для сцены https://elektrokarniz8.ru/ .
Оптимизируйте свою жизнь с электрокарнизом с таймером, удивляйтесь удобству и функциональности.
Создайте атмосферу уюта и стиля с помощью электрокарниза и таймера, добавит функциональности и комфорта.
Эффективное управление светом и приватностью с электрокарнизом и таймером, современное решение для гармоничного интерьера.
Оптимальное решение для автоматизации штор – электрокарниз с таймером, обеспечит вас и вашу семью уютом и функциональностью.
Дизайнерское решение для современного дома – электрокарниз с таймером, позволит вам экономить время и силы.
умные шторы умные шторы .
If you’re looking for a secure and reliable way to download Metamask, I highly recommend checking out https://download.metaredi.org/. Their detailed guide ensures you install it the right way, without any risks.
Управляйте своим окружением с помощью программируемого электрокарниза, подходит для любого окна.
Превратите свой дом в оазис комфорта с программируемым электрокарнизом, который дарит вам полный контроль.
Освежите свою обстановку с помощью программируемого электрокарниза, поможет вам создать идеальный микроклимат.
Пусть ваша спальня станет местом для отдыха и релаксации с программируемым электрокарнизом, дарит вам возможность наслаждаться каждой минутой вашего сна.
Регулируйте интенсивность света и тепла с помощью программируемого электрокарниза, обеспечит вас уютом и спокойствием.
умный дом электрокарниз https://elektrokarniz190.ru/ .
Управляйте своим окружением с помощью программируемого электрокарниза, который легко устанавливается.
Трансформируйте ваше жилище с помощью программируемого электрокарниза, позволяет вам наслаждаться каждой минутой.
Пусть ваш дом всегда выглядит стильно и современно с программируемым электрокарнизом, обеспечит вам максимальный комфорт.
Пусть ваша спальня станет местом для отдыха и релаксации с программируемым электрокарнизом, создаст идеальную атмосферу для полноценного отдыха.
Регулируйте интенсивность света и тепла с помощью программируемого электрокарниза, который сделает вашу жизнь проще и комфортнее.
умный электрокарниз aqara https://elektrokarniz190.ru/ .
I was skeptical about installing the Metamask extension, but after following the guide on https://metamaker.org/#metamask-download, I feel much more confident. Highly recommended for crypto users!
Получите максимум удовольствия от вашего дома с программируемым электрокарнизом, совместим с любым интерьером.
Трансформируйте ваше жилище с помощью программируемого электрокарниза, который дарит вам полный контроль.
Сделайте вашу жизнь проще с программируемым электрокарнизом, который позволит вам сохранить энергию.
Пусть ваша спальня станет местом для отдыха и релаксации с программируемым электрокарнизом, который поможет вам легко заснуть и проснуться.
Регулируйте интенсивность света и тепла с помощью программируемого электрокарниза, поможет вам сэкономить время и энергию.
электрокарниз для умного дома https://elektrokarniz190.ru/ .
Управляйте своим окружением с помощью программируемого электрокарниза, который легко устанавливается.
Трансформируйте ваше жилище с помощью программируемого электрокарниза, позволяет вам наслаждаться каждой минутой.
Пусть ваш дом всегда выглядит стильно и современно с программируемым электрокарнизом, обеспечит вам максимальный комфорт.
Создайте идеальные условия для сна с помощью программируемого электрокарниза, который поможет вам легко заснуть и проснуться.
Создайте идеальные условия для работы и отдыха с программируемым электрокарнизом, обеспечит вас уютом и спокойствием.
электрокарниз для умного дома https://elektrokarniz190.ru/ .
https://answerpail.com/index.php/user/naveridbuy
https://xn--fx-hd0jg6f81ltjas9lbns.mystrikingly.com/blog/4e9937cd8b9
https://naveridbuy.blogspot.com/2024/09/blog-post_19.html
https://diligent-cherry-dc4vld.mystrikingly.com/blog/8d23a06d47d
https://umber-iris-dd3cm2.mystrikingly.com/blog/2
https://xn--jw-o02ik82a9jc69ko8mqkg.mystrikingly.com/blog/e31e874755a
https://telegra.ph/%EB%84%A4%EC%9D%B4%EB%B2%84-%EC%95%84%EC%9D%B4%EB%94%94-%EA%B5%AC%EB%A7%A4%EB%A1%9C-%EC%98%A8%EB%9D%BC%EC%9D%B8-%EC%82%AC%EC%97%85-%EC%8B%9C%EC%9E%91%ED%95%98%EA%B8%B0-07-31-2
https://xn--w2-hd0jg6f81lm0dhhw74c.mystrikingly.com/blog/c1d8850291c
https://ko.anotepad.com/note/read/h5kk7d4j
https://medium.com/@nsw5288/%EB%B9%84%EC%95%84%EA%B7%B8%EB%9D%BC-%EA%B5%AC%EB%A7%A4%EB%A5%BC-%EC%9C%84%ED%95%9C-%EC%8A%A4%EB%A7%88%ED%8A%B8%ED%8F%B0-%EC%95%B1-%EC%B6%94%EC%B2%9C-8acf2b47fedb
https://xn--fc-hd0jg6f81ltjas9lbns.mystrikingly.com/blog/2a1a4a36823
https://maize-wombat-dd3cms.mystrikingly.com/blog/f31a390f699
https://ganghwamarathon.co.kr/bbs/board.php?bo_table=board03_8008&wr_id=261789
Создайте идеальную атмосферу в вашем доме с программируемым электрокарнизом, подходит для любого окна.
Трансформируйте ваше жилище с помощью программируемого электрокарниза, помогает вам расслабиться и отдохнуть.
Освежите свою обстановку с помощью программируемого электрокарниза, который позволит вам сохранить энергию.
Превратите свою спальню в уютное убежище с программируемым электрокарнизом, который поможет вам легко заснуть и проснуться.
Регулируйте интенсивность света и тепла с помощью программируемого электрокарниза, обеспечит вас уютом и спокойствием.
умный электрокарниз алиса умный электрокарниз алиса .
nW7jNmGGFvw
ZWKDknqZG8t
UiYXGvt0kUs
uXAlvohAJLZ
9OLVkKFin3d
2cgurz55neJ
2CIEnHqL2OG
Hp9ZFVpu6bR
rqDIwdtCKsd
M4pmpOuKdJ9
s04BJ7b9oOG
oa3mf6moLnv
YUNKbdhkBhS
DDtGZFp2LWy
JrSEwnLwubl
CVu8EXjHg8g
9vpxqlLg9hY
3yftgd48wPj
JaTaexH9h53
ls9TmGClRxY
7GZqZHPt1I1
N9tNgAhKtYD
zRirA19vQmN
wt0k8bhxBqw
CbovhCfDqQC
5EOa6ckIZj0
gjvcYe07e6o
z0T38Yo6VDp
oOkWG48R4fX
ff5jGF18l58
MEGrdJGITRk
1UNtdFeFW9M
MpYGPXqIbpd
NJS5VYhse5z
nxadmGVDE0N
IOzcTgkGMgl
Ваша сцена станет неповторимой с электрокарнизами, сделают ваше выступление незабываемым.
Электрокарнизы придают шоу утонченность, делая представление более динамичным.
Электрокарнизы для сцены с электронным управлением, дарят возможность воплотить любую идею.
Электрокарнизы помогут создать атмосферу шоу, где каждая деталь важна.
Лучшие электрокарнизы для вашего шоу, с непревзойденным качеством и надежностью.
Сверхсовременные технологии в каждом дизайне, и принести вашему проекту новый уровень.
Уникальные решения для каждого типа представления, которые обеспечат быстрое и плавное движение.
Новейшие электрокарнизы для театральных постановок, и подчеркнуть важность каждой сцены.
Электрокарнизы – современное решение для сцены, с индивидуальным подходом к каждому проекту.
Сотни вариантов электрокарнизов для ваших выступлений, и удивить зрителей нестандартными решениями.
как установить электрокарниз для сцены как установить электрокарниз для сцены .
Through BusinessIraq.com, readers gain access to comprehensive analysis of Iraq’s trade policies, international partnerships, and economic reforms. Our coverage includes detailed reporting on cross-border trade agreements, foreign investment initiatives, and regulatory changes affecting business operations throughout the country.
The Iraqi economy’s transformation receives detailed attention on BusinessIraq.com, with expert analysis of GDP growth, trade balances, and foreign investment flows. Drawing from various economic indicators and market research, we track economic reforms, privatization initiatives, and monetary policy developments. Our coverage extends to international trade agreements, economic partnerships, and cross-border business opportunities that shape Iraq’s economic future.
Анализ финансовых тенденций в Казахстане, находите.
Курс валют в Казахстане сегодня, проверить.
Финансовые отчеты Казахстана: ключевые моменты, чтобы понять ситуацию.
Актуальные экономические тренды Казахстана, подписывайтесь на обновления.
Влияние мировых цен на экономику Казахстана, оценивайте.
Инвестиционные возможности в Казахстане, ознакомьтесь.
Ключи к финансовому успеху в Казахстане, запоминайте.
Что нужно знать о банках Казахстана?, досмотрите.
Что ждет Казахстан в следующем году?, анализируйте.
Изменение налоговой системы в Казахстане, следите.
Какие изменения в денежной политике?, ознакомьтесь.
Как привлечь инвестиции в Казахстане?, узнайте.
Состояние фондового рынка Казахстана, изучайте.
Глобальные тренды и их последствия для Казахстана, ознакомьтесь.
Кредитование в Казахстане: условия и перспективы, читайте.
Актуальные новости о финансовых рынках Казахстана, следите.
Что происходит на рынке недвижимости Казахстана?, ознакомьтесь.
Анализ государственного бюджета Казахстана, изучайте.
Полезные советы по финансам для казахстанцев, проверьте.
Тренды электронных финансов в Казахстане, следите.
финансовые новости Казахстана https://wikibank.kz/ .
As digital transformation sweeps across industries, Iraq Business News covers innovative tech solutions and startups revolutionizing business practices in Iraq’s economic landscape
Are you considering investment opportunities in Iraq? BusinessIraq.com is your gateway to understanding the potential and risks associated with investing in this rapidly evolving market. We provide comprehensive coverage of investment laws, bureaucratic processes, and emerging business sectors ripe for growth. Our articles offer expert analysis on the Iraqi business climate, helping you identify profitable ventures and navigate potential challenges. From infrastructure projects to agricultural advancements, we highlight potential areas of high return, offering a nuanced perspective on both the opportunities and risks in various sectors. Learn about accessing funding, partnering with local businesses, and understanding the cultural nuances that impact the investment process.
Its like you read my mind You appear to know so much about this like you wrote the book in it or something I think that you can do with a few pics to drive the message home a little bit but instead of that this is excellent blog A fantastic read Ill certainly be back
Using MetaMask Extension every day. It makes interacting with smart contracts super simple. Highly recommended for DeFi enthusiasts!
hentairead Nice post. I learn something totally new and challenging on websites
Mitolyn I just like the helpful information you provide in your articles
Puraburn This was beautiful Admin. Thank you for your reflections.
MetaMask Download is fast and efficient. Setting up a wallet is easy, and the interface is designed for all levels of users.
MetaMask Download made easy! Setting up a wallet takes minutes, and it’s perfect for managing Ethereum and NFTs effortlessly.
neuroprime scam: neuroprime scam
neuroprime scam: neuroprime scam
denticore scam: denticore scam
arctic blast scam: arctic blast scam
Your blog is a true hidden gem on the internet. Your thoughtful analysis and engaging writing style set you apart from the crowd. Keep up the excellent work!
Gluco6 scam: Gluco6 scam
Pineal Guardian scam: Pineal Guardian scam
FemiPro scam: FemiPro scam
Java Burn scam: Java Burn scam
Quietum Plus scam: Quietum Plus scam
Your positive and uplifting words are like a ray of sunshine on a cloudy day Thank you for spreading light and positivity in the world
Puraburn Hi there to all, for the reason that I am genuinely keen of reading this website’s post to be updated on a regular basis. It carries pleasant stuff.
MetaMask Chrome provides great flexibility. Supports various blockchains and allows easy token swapping. A fantastic tool for crypto users.
MetaMask Download is a smart move for investors. Keeping assets safe while accessing blockchain networks has never been easier.
Veryy nice blog post. I certainly lovge thks site. Stiick with it!
MetaMask Download is a must for Web3. The interface is user-friendly, and it allows seamless access to decentralized applications.
Sitedeki tüm profiller özenle seçilmiş, fotoğraflar gerçek ve tutarlı. Özellikle Ankara escort arayanlar için güvenli bir ortam sunuyor.
Идеальные шторы под заказ
пошив штор на заказ пошив штор на заказ .
Закажите уникальные шторы на заказ, для офиса.
Качественные шторы на заказ, по выгодной цене.
Изготовление штор на заказ, под любой стиль.
Эксклюзивные шторы на заказ, высокое качество материалов.
Пошив штор на заказ для кухни, с индивидуальным подходом.
Надежное изготовление штор на заказ, по вашим желанием.
Создание штор на заказ из натуральных тканей, используя современные технологии.
Эксклюзивные шторы на заказ, подчеркивающие вашу индивидуальность.
Классические шторы на заказ, под любой интерьер.
Создание штор для любого типа окна, от ведущих мастеров.
Креативные шторы на заказ, под любой интерьер.
Изготовление штор на заказ быстро и недорого, с высоким качеством.
Элегантные шторы на заказ, под любой стиль интерьера.
Дизайнерские шторы на заказ, по вашему проекту.
Пошив штор по индивидуальному дизайну, от профессиональных мастеров.
Эксклюзивные ткани для пошива штор, под любой стиль.
сшить шторы на заказ сшить шторы на заказ . Прокарниз
Эксклюзивные римские шторы по вашим размерам
римские шторы на заказ римские шторы на заказ .
Креативные идеи штор для загородного дома
шторы в загородном доме шторы в загородном доме .”Ткацкий”
Sitedeki tüm içerikler SEO uyumlu ve kullanıcıyı yanıltmıyor. Ankara escort arayan herkes için güvenilir bir kaynak.
SIGMASLOT : Situs Slot Online Terpercaya untuk Menang Besar
SIGMASLOT : Situs Slot Online Terpercaya untuk Menang Besar
SIGMASLOT : Situs Slot Online Terpercaya untuk Menang Besar
Умные деревянные жалюзи с электроприводом
Деревянные горизонтальные жалюзи с электроприводом Деревянные горизонтальные жалюзи с электроприводом . прокарниз
MetaMask Extension has made my crypto journey smoother. Secure and fast transactions make it an excellent choice for users.
Get ready to elevate your betting experience with an exclusive 1xBet promo code! Whether you’re from Bangladesh, Pakistan, India, Nepal, Sri Lanka, Nigeria, Egypt, or the Philippines, you can unlock amazing rewards like free bets, no deposit bonuses, and free spins using the latest 1xBet promo codes today. New users can enjoy a special registration promo code that boosts your first deposit or even gives you a chance to play risk-free. Looking for a Bangladesh 1xBet promo code or a 1xBet promo code India for the app? We’ve got it all here, updated daily. Don’t miss your chance to grab a 1xBet official promo code, win big, and make the most out of your betting journey. Claim your 1xBet free promo code today and start winning smarter with bigger bonuses, free spins, and more exclusive offers worldwide! No matter where you are, finding the right 1xBet promo code today means unlocking bigger chances to win, with offers perfectly tailored for players across Bangladesh, Pakistan, India, Nepal, Sri Lanka, Nigeria, Egypt, and the Philippines.
Получить онлайн консультацию психолога чате. Психолог онлайн анонимно. В переписке у психолога.
Консультация в кризисных состояниях.
Сколько встреч нужно?
Индивидуальное консультирование.
Онлайн сессия от 91777 руб.
Личные или онлайн-встречи с высококвалифицированными специалистами.
Психологическая помощь онлайн.
Получить онлайн консультацию психолога чате. Получите консультацию онлайн-психолога в чате прямо сейчас. Психолог онлайн анонимно.
Эмоциональное состояние: тревога, депрессия, стресс, эмоциональное выгорание.
Задайте интересующие вас вопросы или запишитесь на сеанс к психологу.
Получить поддержку по широкому кругу вопросов.
аккаунт для рекламы магазин аккаунтов
магазин аккаунтов социальных сетей площадка для продажи аккаунтов
платформа для покупки аккаунтов аккаунт для рекламы
маркетплейс аккаунтов https://ploshadka-prodazha-akkauntov.ru/
магазин аккаунтов https://prodat-akkaunt-online.ru/
маркетплейс для реселлеров услуги по продаже аккаунтов
маркетплейс аккаунтов https://pokupka-akkauntov-online.ru/
Account Catalog https://buyverifiedaccounts001.com
Account Trading Social media account marketplace
Account market Online Account Store
Accounts for Sale Account Buying Service
Social media account marketplace Account Buying Service
Account Market Sell Pre-made Account
Account Exchange Service Sell Pre-made Account
Ready-Made Accounts for Sale Gaming account marketplace
Online Account Store Buy Account
Accounts marketplace Social media account marketplace
secure account purchasing platform gaming account marketplace
accounts market account trading
account exchange verified accounts for sale
Онлайн-консультация психолога. Анонимный чат с психологом телеграм. Психолог в телеграм.
Эмоциональное состояние: тревога, депрессия, стресс, эмоциональное выгорание.
Индивидуальное консультирование.
Поможет поставить цель терапии и приведет к результату.
account selling service purchase ready-made accounts
Онлайн чат с психологом без регистрации. Психологическая и информационная онлайн-помощь. Психолог онлайн анонимно.
94195 проверенных отзывов.
Правильно оценить происходящее в жизни и найти выход из сложившейся жизненной ситуации.
Анонимный прием.
account store accounts market
account sale account buying service
buy pre-made account accounts for sale
account trading secure account sales
account purchase online account store
sell pre-made account profitable account sales
social media account marketplace account trading platform
account market account exchange
online account store secure account purchasing platform
account catalog website for selling accounts
account catalog sell pre-made account
account exchange service account market
sell pre-made account account purchase
Задать вопрос психологу. Психолог онлайн чат. Psychologue.
Индивидуальное консультирование.
Сколько встреч нужно?
Психолог владеет множеством приемов и техник, которые помогут разобраться в себе.
Личные или онлайн-встречи с высококвалифицированными специалистами.
account trading service account sale
buy pre-made account account catalog
find accounts for sale account purchase
accounts marketplace account exchange service
account purchase guaranteed accounts
account acquisition buy accounts
secure account sales account exchange service
profitable account sales account store
verified accounts for sale marketplace for ready-made accounts
accounts for sale database of accounts for sale
website for buying accounts profitable account sales
guaranteed accounts accounts marketplace
account trading platform https://accounts-marketplace.xyz
buy pre-made account accounts market
account buying platform https://social-accounts-marketplaces.live/
account selling platform https://accounts-marketplace.live
website for buying accounts https://social-accounts-marketplace.xyz
verified accounts for sale account marketplace
account acquisition https://buy-accounts-shop.pro
account selling platform https://buy-accounts.live/
account exchange service https://social-accounts-marketplace.live
account marketplace https://accounts-marketplace.online/
Психотерапевт онлайн чат. Анонимный чат с психологом телеграм. Чат анонимный.
Нужен хороший психолог?
Запись на прием, оплата, подробная информация о специалистах и отзывы клиентов.
Решим вместе вашу проблему.
Анонимный прием.
accounts market accounts market
продажа аккаунтов https://akkaunty-na-prodazhu.pro
биржа аккаунтов rynok-akkauntov.top
площадка для продажи аккаунтов https://kupit-akkaunt.xyz
В переписке у психолога. Психотерапевт онлайн чат. Сайты психологов.
Личные или онлайн-встречи с высококвалифицированными специалистами.
Эмоциональное состояние: тревога, депрессия, стресс, эмоциональное выгорание.
Мы обязательно поможем преодолеть эмоциональный кризис, избавиться от тревожности и апатии, справиться со стрессом и депрессией, связанными с неуверенностью и многим другим.
Психологическая поддержка онлайн чат. Психолог спб отзывы. Психологи онлайн.
Получить поддержку по широкому кругу вопросов.
Нужен хороший психолог?
Решим вместе вашу проблему.
Эмоциональное состояние: тревога, депрессия, стресс, эмоциональное выгорание.
маркетплейс аккаунтов соцсетей https://akkaunt-magazin.online
продать аккаунт https://akkaunty-market.live
магазин аккаунтов kupit-akkaunty-market.xyz
Онлайн разговор с психологом. Получите помощь психолога онлайн. Помощь психолога онлайн.
Запись на прием, оплата, подробная информация о специалистах и отзывы клиентов.
Психолог Москва. Психолог СПБ. Психолог онлайн.
Психологическая помощь онлайн.
биржа аккаунтов https://akkaunty-optom.live
купить аккаунт https://online-akkaunty-magazin.xyz/
площадка для продажи аккаунтов https://akkaunty-dlya-prodazhi.pro
биржа аккаунтов kupit-akkaunt.online
Найти психолога онлайн. Помощь психолога онлайн чат. Мне нужен хороший психолог.
Психологическое консультирование.
Задайте интересующие вас вопросы или запишитесь на сеанс к психологу.
Услуги психолога · — Консультация психолога.
buy fb ad account https://buy-adsaccounts.work
buy accounts facebook facebook ad account buy
facebook ad account for sale https://buy-ad-account.top
Психолог онлайн чат. Помощь психолога онлайн. Психолог онлайн.
Личные или онлайн-встречи с высококвалифицированными специалистами.
Психологическое консультирование заключается в том, чтобы помочь клиенту разобраться в своих проблемах и вместе с ним найти пути выхода из сложной ситуации.
Сколько встреч нужно?
Решим вместе вашу проблему.
buy facebook old accounts https://buy-ads-account.click
Психолог онлайн 24. Psicologo. Онлайн общение с психологом.
Психолог владеет множеством приемов и техник, которые помогут разобраться в себе.
Решим вместе вашу проблему.
Записаться на консультацию.
Запись на прием, оплата, подробная информация о специалистах и отзывы клиентов.
facebook accounts to buy facebook account buy
buy fb ad account facebook ad account buy
buy facebook account for ads buy facebook accounts for ads
Психотерапия по переписке. Психологи онлайн анонимно. Анонимный психолог.
Запись на прием, оплата, подробная информация о специалистах и отзывы клиентов.
Психолог Москва. Психолог СПБ. Психолог онлайн.
60199 проверенных отзывов.
Эта статья для ознакомления предлагает читателям общее представление об актуальной теме. Мы стремимся представить ключевые факты и идеи, которые помогут читателям получить представление о предмете и решить, стоит ли углубляться в изучение.
Узнать больше – https://medalkoblog.ru/
cheap facebook accounts facebook account buy
buy account facebook ads https://ad-accounts-for-sale.work
buy google adwords accounts https://buy-ads-account.top
Психолог онлайн анонимно. Психолог Ялта Задать вопрос психологу.
Психологическая помощь онлайн.
Записаться на консультацию.
Онлайн сессия от 5041 руб.
buy verified google ads accounts buy verified google ads account
buy facebook ad account facebook ad account buy
buy google ads account https://ads-account-for-sale.top/
buy google ads threshold account buy google ads agency account
google ads accounts for sale https://buy-ads-invoice-account.top
buy adwords account buy google adwords account
buy verified google ads accounts buy google ads agency account
google ads reseller google ads account buy
buy google ads verified account https://ads-agency-account-buy.click
buy verified facebook https://buy-business-manager.org/
buy verified google ads account buy aged google ads account
buy fb bm buy-bm-account.org
buy business manager account facebook bm buy
buy facebook ads accounts and business managers buy-verified-business-manager-account.org
buy fb bm https://buy-verified-business-manager.org
buy facebook business manager accounts https://business-manager-for-sale.org
facebook bm account facebook bm account
buy facebook verified business manager https://buy-bm.org/
verified bm for sale https://verified-business-manager-for-sale.org/
buy verified bm facebook https://buy-business-manager-accounts.org/
buy tiktok ads accounts https://buy-tiktok-ads-account.org
tiktok agency account for sale https://tiktok-ads-account-buy.org
tiktok agency account for sale https://tiktok-ads-account-for-sale.org
tiktok ad accounts https://tiktok-agency-account-for-sale.org
tiktok agency account for sale https://buy-tiktok-ad-account.org
buy tiktok ads https://buy-tiktok-ads-accounts.org
Помощь психолога анонимно. Психолог Ялта Психологи онлайн.
Получить поддержку по широкому кругу вопросов.
Личные или онлайн-встречи с высококвалифицированными специалистами.
Поможет поставить цель терапии и приведет к результату.
Онлайн сессия от 57634 руб.
tiktok ads agency account https://tiktok-ads-agency-account.org
tiktok ads account buy https://buy-tiktok-business-account.org
buy tiktok business account https://buy-tiktok-ads.org
Thanks, Ample content.
Wow that was odd. I just wrote an very long comment but after I clicked submit my comment didn’t show up. Grrrr… well I’m not writing all that over again. Anyway, just wanted to say excellent blog!
https://blogfreely.net/bikepaint3/partying-the-legacy-regarding-henry-thierry-often-known-as-thierry-anri
кайт египет
Heya outstanding website! Does running a blog similar to this take a massive amount work? I’ve no knowledge of computer programming however I had been hoping to start my own blog in the near future. Anyhow, if you have any suggestions or techniques for new blog owners please share. I understand this is off topic but I just wanted to ask. Thank you!
https://curry-bendtsen-2.hubstack.net/rafael-nadal-rolan-garrosyn-unemlekhui-khaan-uu
cialis compresse 5 mg prezzo : a medication containing tadalafil, treats erectile dysfunction and benign prostatic hyperplasia. In Italy, a 28-tablet pack of Cialis 5 mg costs approximately €165.26, but costs differ by pharmacy and promotions. Generic alternatives, like Tadalafil DOC Generici, range from €0.8–€2.6 per tablet, providing a budget-friendly option. Always consult a doctor, as a prescription is needed.
кайт сафари
Hi there, You’ve done an excellent job. I’ll certainly digg it and personally suggest to my friends. I’m sure they’ll be benefited from this site.
https://brightwallpapers.com.ua/yak-vidriznyty-oryhinalnyy-elektroshoker-vid-pidroblenoho-porady-ta-rekomendatsiyi
кайтинг
https://www.med2.ru/story.php?id=147093
Психологическая помощь онлайн анонимно. Психолог Москва Онлайн чат с людьми.
Решим вместе вашу проблему.
Раздражительность на членов своей семьи.
Запись на прием, оплата, подробная информация о специалистах и отзывы клиентов.
https://oboronspecsplav.ru/
Пассажирские перевозки Томск – Экибастуз Развитая сеть пассажирских перевозок играет ключевую роль в обеспечении мобильности населения и укреплении экономических связей между регионами. Наша компания специализируется на организации регулярных и безопасных поездок между городами Сибири и Казахстана, предлагая комфортные условия и доступные цены.
Психологическая поддержка онлайн. Психолог по личным отношениям. Psychologue.
Онлайн сессия от 46654 руб.
Частые разногласия с самыми близкими.
Психологическое консультирование.
«Рентвил» предлагает аренду автомобилей в Краснодаре без залога и ограничений по пробегу по Краснодарскому краю и Адыгее. Требуется стаж от 3 лет и возраст от 23 лет. Оформление за 5 минут онлайн: нужны только фото паспорта и прав. Подача авто на жд вокзал и аэропорт Краснодар Мин-воды Сочи . Компания работает 10 лет , автомобили проходят своевременное ТО. Доступны детские кресла. Бронируйте через сайт авто в аренду краснодар
поставки товара из Китая В эпоху глобализации и стремительного развития мировой экономики, Китай занимает ключевую позицию в качестве крупнейшего производственного центра. Организация эффективных и надежных поставок товаров из Китая становится стратегически важной задачей для предприятий, стремящихся к оптимизации затрат и расширению ассортимента. Наша компания предлагает комплексные решения для вашего бизнеса, обеспечивая бесперебойные и выгодные поставки товаров напрямую из Китая.
Шкаф Кухня – сердце дома, место, где рождаются кулинарные шедевры и собирается вся семья. Именно поэтому выбор мебели для кухни – задача ответственная и требующая особого подхода. Мебель на заказ в Краснодаре – это возможность создать уникальное пространство, идеально отвечающее вашим потребностям и предпочтениям.
This school model looks promising: https://nordicinternationalschool.pk/art/democratic_education_the_future.html
В динамичном мире Санкт-Петербурга, где каждый день кипит жизнь и совершаются тысячи сделок, актуальная и удобная доска объявлений становится незаменимым инструментом как для частных лиц, так и для предпринимателей. Наша платформа – это ваш надежный партнер в поиске и предложении товаров и услуг в Северной столице. Строительная доска объявлений
аккаунт варфейс В мире онлайн-шутеров Warface занимает особое место, привлекая миллионы игроков своей динамикой, разнообразием режимов и возможностью совершенствования персонажа. Однако, не каждый готов потратить месяцы на прокачку аккаунта, чтобы получить желаемое оружие и экипировку. В этом случае, покупка аккаунта Warface становится привлекательным решением, открывающим двери к новым возможностям и впечатлениям.
инди музыка Роп – Русский роп – это больше, чем просто музыка. Это зеркало современной российской души, отражающее её надежды, страхи и мечты. В 2025 году жанр переживает новый виток развития, впитывая в себя элементы других стилей и направлений, становясь всё более разнообразным и эклектичным. Популярная музыка сейчас – это калейдоскоп звуков и образов. Хиты месяца мгновенно взлетают на вершины чартов, но так же быстро и забываются, уступая место новым музыкальным новинкам. 2025 год дарит нам множество талантливых российских исполнителей, каждый из которых вносит свой неповторимый вклад в развитие жанра.
Профили в Дизайне человека · 1 линия — Исследователь · 2 линия — Отшельник · 3 линия — Мученик · 4 линия — Опортунист · 5 линия — Еретик · 6 линия — Ролевая модель. Ворота 52
12 профилей в Дизайне человека. Исследователь. Отшельник. Мученик. Оппортунист. Еретик. Ролевая модель.
Дизайн человека помогает понять, какой тип энергии вы излучаете, как вы принимаете решения, и как лучше использовать свою энергию, чтобы не выгорать, а чувствовать себя более удовлетворённым
Для каждого человека естественного искать выгоду для себя. Так происходит и с Дизайном Человека.